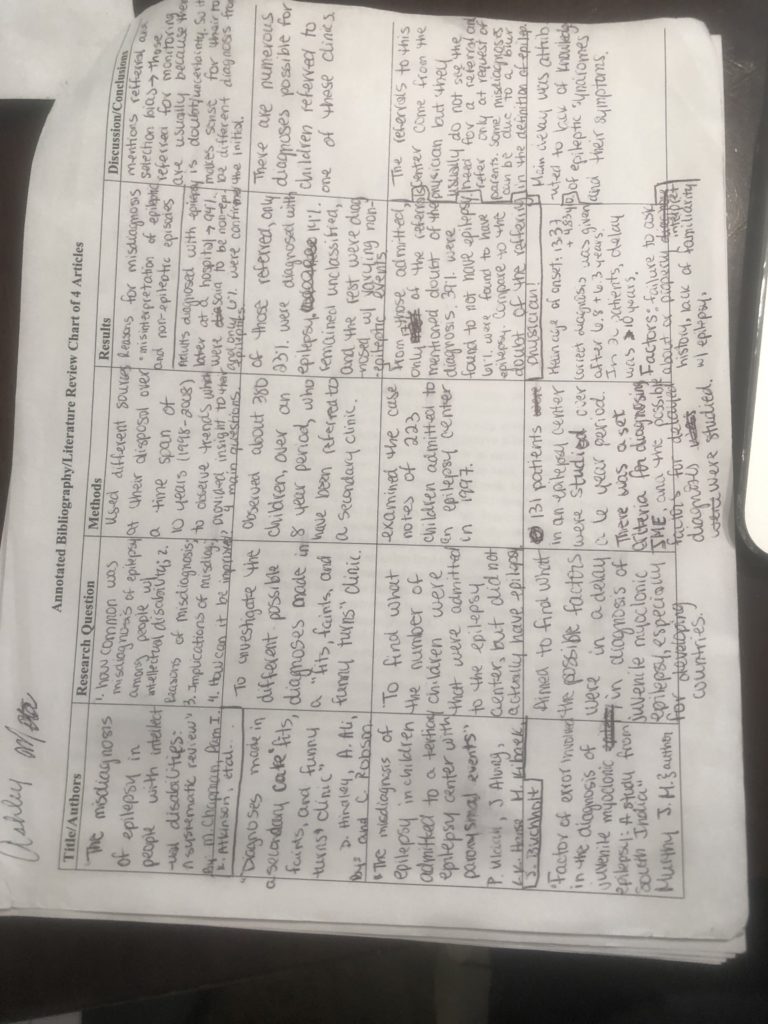
This assignment was a Literature Review. I chose the topic of “misdiagnosis of epilepsy” after I was it mentioned in a pediatric journal. In this assignment I reviewed 4 different articles to explore the main factors which led to the common misdiagnosis of epilepsy. Once I found the main components listed, in nearly all of the articles, I chose those factors as the subheadings for the Analysis portion of the paper. Analysis of those factors allowed for an inference to what the solution to the problem of misdiagnosing epilepsy, which was the basis of the conclusion.
Factors
Resulting in the Misdiagnosis of Epilepsy: A Literature Review
ABSTRACT
The
condition of epilepsy is one that has many different symptoms and is commonly
misdiagnosed. Epilepsy misdiagnosis can be seen through labeling a
non-epileptic condition as epilepsy or an epileptic condition being labeled as
being non-epileptic. The major factors leading to misdiagnosis are 1) confusion
between epileptic symptoms and non-epileptic episodes, 2) misinterpretation of
the results from different clinical tests such as EEGs and MRIs, and 3) the lack
of referral to epileptic centers based on the certainty of doctors in their
initial diagnoses. The misdiagnosis of epilepsy has a major implication for the
treatment which patients receive- in which they might be getting inappropriate
treatment for a condition they do not possess. A possible solution to lessen
the extent to which epilepsy is misdiagnosed can be to always refer
epileptic-like cases to a center which specializes in epilepsy, so that a
diagnosis is more accurate.
INTRODUCTION
Epilepsy is a serious condition which has
different symptoms, among which seizure is the most common. The disturbance in
brain activity that is caused by the symptoms of epilepsy can be harmful to the
body and brain. Therefore, once an epileptic diagnosis is made, actions for
treatment should be taken right away. Treatment for epilepsy can be different
anti-epilepsy medication. While epilepsy is a very serious condition, there are
accounts of common misdiagnosis of epilepsy. Misdiagnosis of epilepsy can be seen
in two forms: one is diagnosing a condition as epilepsy, when it is not, or
diagnosing another condition when it is epilepsy. In this literature review, a
different number of studies will be analyzed and compared to target which
factors contribute to the common misdiagnosis of epilepsy. The aim is to
pinpoint those factors and identify a possible solution so that the rate of
misdiagnosis can be reduced. This topic is of great importance because a
misdiagnosis of epilepsy can have many undiscovered implications for the
patient receiving the wrong diagnosis. When thinking of the importance of treatment
for epilepsy, a possible implication of misdiagnosis is that a person will not
receive the proper treatment for the treatment they possess- whether it be
epilepsy or another condition. Additionally, a person can be treated for an
illness they do not have and experience unknown side effects. With the analysis
of the main factors leading to the misdiagnosis of epilepsy, the implications
can be known, and a possible solution can be established.
ANALYSIS
Common Non-Epileptic Events and Symptoms Confused with Epilepsy
There are many different
diagnosis possibilities that can be assigned to symptoms common to epilepsy,
among which some were syncope, migraines, daydreaming, night terrors, psychological
episodic spells, tics, staring, dystonia, and disturbances during sleep (Hindley
et al 2006; Uldall et al 2006). Syncope is the most common non-epileptic event
that is mistaken with epilepsy (Hindley et al 2006; Fattouch et al 2007). Two
of the most notable differences between epileptic events and non-epileptic
events were that non-epileptic events were situational, meaning that they were
triggered by a specific event or activity, and that non-epileptic episodes
could be interrupted (Hindley et al 2006).This shows that even if symptoms seem
to be the same for epileptic and non-epileptic episodes, there are other factors
that could come into play which could aid in differentiating the two. Fattouch (2007)
supported this idea with the use of a questionnaire and scoring system that differentiated
between epileptic seizures and syncope. The questionnaire asked different
questions and each question had a specific scoring where it added points or
subtracted points. Some of the questions were if there was unresponsiveness
during the spell, if there was sweating before the spell, and if the spell was
associated with prolonged sitting or standing. The question regarding unresponsiveness
during a spell gets a point, going towards the characteristics of an epileptic
seizure, and sweating before a spell or the spell being caused by prolonged
sitting or standing loses two points, going away from epileptic seizure and
moving towards a syncope diagnosis. These three characteristics depict examples
of how to distinguish between non-epileptic and epileptic spells using two of
the differentiating factors expressed by Hindley (2006).
These cases dealt
with an epileptic diagnosis being given to non-epileptic events. However, the
reverse can happen as well. The lack of knowledge regarding the symptoms of
epilepsy can lead to an improper diagnosis of an actual epileptic episode. In
other words, symptoms might be labeled as being non-epileptic when in reality
the patient possesses epilepsy. Murthy (1999) conducted a study for the factors
leading to delay in diagnosis of Juvenile Myoclonic Epilepsy (JME) in South
India with 131 patients. The symptoms for JME are explicitly known; however,
the time span in which they appear can vary between each other. For example,
generalized tonic clonic seizures (GTCS) are often the first symptoms to appear
but the circadian relations to awakening from sleep might not be fully
manifested right away. Additionally, the appearance of absence seizures can
precede GTCS and myoclonic jerks by 4 to 5 years. If a doctor is unaware of the
time span and characteristics of the symptoms of JME, they might just give a
diagnosis of absence epilepsy and not even consider JME as a potential future
problem. If the contrasts between non-epileptic episodes and specific epileptic
seizures are not very well known, there can be an effect on the diagnosis given
to a patient.
Misinterpretation of Data: EEGs, MRI, Etc.
When in centers that
do not specialize in epilepsy, it is hard to accurately analyze the data
collected through different tests in order to give the proper diagnosis (Britton
2004 cited by Fattouch et al 2007; Uldall et al 2006). The study conducted by Fattouch et al (2007)
had a cohort of 62 subjects, 57 of which were found to have a definite
diagnosis of syncope. They were divided up into two groups to further analyze
their data accordingly. 30 of the patients had received a “definite epileptic”
diagnosis; they made up the syncopes misdiagnosed as epileptic seizures (SMS)
group. 27 of the patients were only suspected
of having epilepsy; these individuals were labeled as unrecognized syncopes
(US). 70% of the SMS patients showed abnormal EEGs and 37% showed some
alteration in their MRI findings. In the US group, 33% had EEG abnormality and
only 1 had an MRI alteration. These statistics showed that there were abnormal
results collected from the MRI and EEGs, however, all of the subjects had a
syncope diagnosis, despite those abnormalities.
Similarly, in
Hindley’s (2006) study, of 380 subjects, there were differing abnormalities found.
Abnormalities were reported in 84%
of the subject count. Of this group, 85% of them were abnormal at the first
testing, but for 15% a repeat EEG, sleep EEG, or prolonged EEG was required. This
showed that due to uncertainty, a second testing might be needed for established
accuracy. 53% of the entire subject
population had computed tomography (CT) scans, out of which 23% showed some type
of abnormality. 52% had magnetic resonance imaging (MRI) scans, and 41% of this
group showed abnormality. The large presence of abnormalities could have misled
an epileptic diagnosis. However, only 23% of the subject population was
actually confirmed to have an epilepsy diagnosis.
This shows that
some doctors might be tricked by those abnormalities thinking that they point
directly to an epileptic characteristic of EEGs and MRIs. However, a proper
analysis is required to be able to distinguish between abnormal syncope, or
other non-epileptic events, results and definite epileptic results.
Doctors’ Certainty of Diagnosis:
The certainty of a
doctor on the diagnosis they are giving can deter from the proper steps being
taken to reach confirmation of an intended diagnosis. Some doctors
underestimate symptoms because they don’t want to give a harsh diagnosis such
as epilepsy for symptoms, which they are unclear of, to then have to retract
it. So, they prefer to label it as not being epilepsy, and then correct it
after the fact. (O’Donohoe 1994
cited by Hindley 2006) In Uldall’s (2006) et al study, 223 children were
observed, 17% of them had referrals where their doctor had doubt about their
epileptic diagnosis. From these uncertain referrals, 18% had confirmed epilepsy
and 82% did not have confirmed epilepsy. These doctors, worked similar to what
Hindley talked about, showing that it was better to have a non-epileptic or
uncertain diagnosis to then have it corrected. In contrast to this idea,
Uldall’s (2006) study also had 83% of their subject population with referrals
where their doctors were “without a doubt” certain of their epileptic diagnosis.
From these, 70% had a confirmed epileptic diagnosis and 30% did not actually
have epilepsy. The referrals from these doctors came mostly at the request of
parents. This shows that doctor’s could have such a strong feeling about their
epileptic diagnosis, despite their equipment and setting being inferior to that
of the epileptic centers, that 30% of patients would have been dismissed with
the wrong diagnosis. This is the perfect depiction of when the certainty of a
doctor could negatively impact the misdiagnosis of epilepsy.
CONCLUSION
When dealing with the diagnosis of
epilepsy, it is important to take into consideration the different symptoms and
possible non-epileptic diagnoses, as well as accurately decipher the clinical
data before a final diagnosis is made (Murthy 1999; Hindley et al 2006; Uldall
et al 2006; Fattouch et al 2007). Additionally, doctors should never be too
certain in their diagnosis, especially one that was made outside of an
epileptic center. Since major factors
established to affect misdiagnosis of epilepsy are often present in areas not specialized for epilepsy, it can be
inferred that a proposed solution to the misdiagnosis
of epilepsy is the referral of any episodes that even seemingly resemble
epilepsy to epilepsy centers before an epilepsy diagnosis is made (Murthy 1999; Hindley
et al 2006; Uldall et al 2006; Fattouch et al 2007). The major implications for
the misdiagnosis of epilepsy can be a delay in appropriate treatment for the
proper condition. The exact side effects of receiving treatment for the wrong
condition was not explored by these researchers; therefore, that is an area for
possible future directions in this topic.
References:
Fattouch J., Di Bonaventura C.,
Strano S., Vanacore N., Manfredi M., Prencipe M., Giallonardo A.T. 2007.
Over-interpretation of electroclinical and neuroimaging findings in syncope
misdiagnosed as epileptic seizures. Epileptic Discord. 9(2)(170-173)
[Internet][Accessed May 8 2019]
Available from: https://pdfs.semanticscholar.org/d2f5/2e5e508d5cb5fbae52f1d0256a4759220345.pdf
Hindley D., Ali A., Robson C. 2006.
Diagnoses made in a secondary care “fits, faints, and funny turns” clinic. ADC.
91(3)(214-218). [Internet] [Accessed April 15 2019]
Available from: https://adc-bmj-com.clinical-proxy.libr.ccny.cuny.edu/content/91/3/214
Murthy JM. 1999. Factors of error
involved in the diagnosis of juvenile myoclonic epilepsy: a study from South
India. Neurology India. 47(3)(210-213). [ Internet] [Accessed April 13 2019]
Available from: http://www.neurologyindia.com/article.asp?issn=0028-3886;year=1999;volume=47;issue=3;spage=210;epage=3;aulast=murthy
Uldall P., Alving J., Hansen L K.,
Kibaek M., Buchholt J. 2006. The misdiagnosis of epilepsy in children admitted
to a tertiary epilepsy centre with paroxysmal events. ADC. 91(3)(219-221).
[Internet] [Accessed April 10 2019]
Available from: https://adc-bmj-com.clinical-proxy.libr.ccny.cuny.edu/content/91/3/219